Basal cell skin cancer is a type of skin cancer that originates in the basal cells, a type of skin cell responsible for regenerating new skin. Cancer develops after DNA mutations occur, appearing as a lesion. There are several basal cell skin cancer causes to be aware of — and many are preventable. Protect yourself and your skin with these tips from GentleCure.
Basal Cell Skin Cancer Causes
What causes basal cell skin cancer? The biggest risk factors are sunlight exposure and ultraviolet radiation present in tanning beds. Too much light can cause DNA mutations that interrupt the basal cell’s regular cell production, leading to rapid cell development that’s too much for the body to handle. Rather than the routine cycle of cells being pushed to the skin’s surface where they eventually slough off and die, the overabundance of cells get trapped, becoming a cancerous tumor and causing other symptoms.
Sunlight and UV are not the only risk factors to consider. Below we’ll go over some of the risk factors that can cause BCC.
Risk Factors of Basal Cell Skin Cancer
Several factors contribute to what causes basal cell skin cancer, each playing a significant role in the likelihood of its occurrence:
- Prolonged Sun Exposure: Spending long periods under the sun’s harmful ultraviolet (UV) rays increases the risk of basal cell skin cancer. Over time, cumulative exposure to UV radiation damages the DNA in skin cells, leading to abnormal growth and potential cancer development.
- History of Sunburns: Sunburns, especially during childhood or adolescence, are a significant risk factor for basal cell skin cancer. Intense or frequent sunburns can cause lasting damage to the skin, predisposing individuals to skin cancer later in life.
- Fair Skin: People with fair skin, light hair, and light-colored eyes are at higher risk of developing basal cell skin cancer. Fair-skinned individuals have less melanin, a pigment that helps protect the skin from UV radiation. As a result, they are more susceptible to sun damage and skin cancer.
- Family History of Skin Cancer: A family history of skin cancer, including basal cell skin cancer, increases the likelihood of developing the disease. Genetic factors can play a role in susceptibility to skin cancer, and individuals with relatives who have had skin cancer may have an elevated risk themselves.
- Weakened Immune System: A compromised immune system, whether due to medical conditions like HIV/AIDS, organ transplantation, or immunosuppressive medications, can raise the risk of basal cell skin cancer. A weakened immune system may be less effective at detecting and destroying abnormal cells, allowing cancer to develop more easily.
Understanding these risk factors is essential for individuals to assess their susceptibility to basal cell skin cancer and take appropriate preventive measures. Practicing sun safety, including wearing protective clothing, using sunscreen, seeking shade, and avoiding tanning beds, can help mitigate the risk of developing this common form of skin cancer. Additionally, individuals with a higher risk profile should prioritize regular skin screenings and consult with healthcare providers for personalized recommendations on skin cancer prevention and early detection strategies.
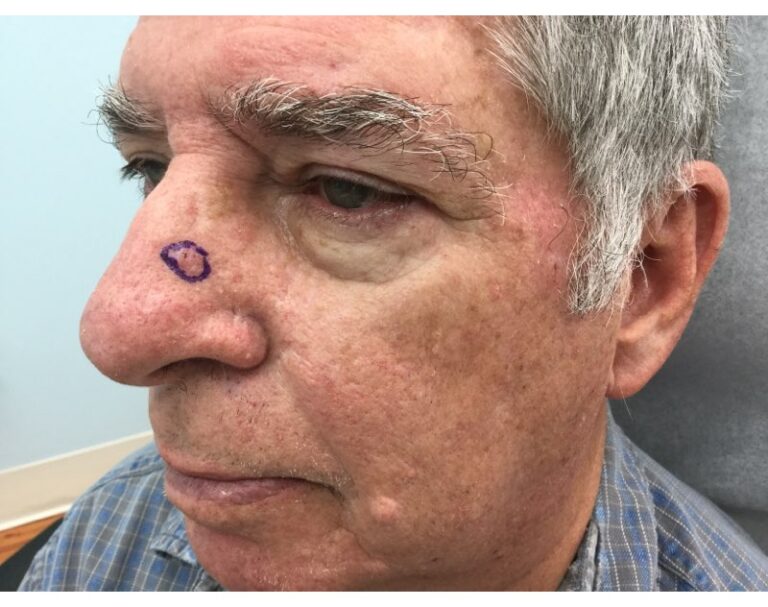
Identifying Basal Cell Skin Cancer
Knowing what causes basal cell skin cancer is one thing, but identifying it early can be vital for you or your loved ones. Basal cell skin cancer is the most common form of skin cancer, affecting millions of people worldwide. While it’s highly treatable, early detection is key to successful treatment. Understanding the signs and symptoms of basal cell skin cancer can empower you to take proactive steps toward your skin health. Here are some things to keep in mind when learning how to tell if it’s basal cell skin cancer or not:
- Unusual Growth or Change: Keep an eye out for any unusual growths or changes on your skin. Basal cell skin cancer often appears as a pearly or waxy bump, a flat, flesh-colored or brown scar-like lesion, or a pinkish patch of skin. These growths may bleed easily or develop a crust or scab.
- Slow-Growing Lesions: Basal cell skin cancer typically grows slowly over time. Pay attention to any persistent sores or spots that don’t seem to heal, as these may be indicative of basal cell skin cancer.
- Changes in Appearance: Basal cell skin cancer lesions can change in appearance over time. Watch for any changes in size, shape, color, or texture of existing moles or growths on your skin. Additionally, be mindful of any new growths that appear suddenly.
- Location: Basal cell skin cancer commonly occurs on areas of the skin that are frequently exposed to the sun, such as the face, ears, neck, scalp, shoulders, and back. However, it can develop on any part of the body, including areas that are not regularly exposed to sunlight.
If you notice any suspicious changes on your skin or experience any concerning symptoms, it’s essential to consult a dermatologist promptly. A dermatologist can perform a thorough examination of your skin, diagnose any abnormalities, and recommend appropriate treatment options.
ABCDEs of Skin Cancer
Understanding the ABCDEs of skin cancer is crucial for early detection, including how to tell if it’s BCC. Each letter represents a key visual sign associated with the disease:
- A – Asymmetry: One half of the mole or spot doesn’t match the other half, indicating irregularity.
- B – Border: The borders of a mole are irregular, jagged, or poorly defined.
- C – Color: The mole has uneven coloring, with shades of brown, black, tan, red, white, or blue.
- D – Diameter: The mole’s diameter is larger than a pencil eraser (approximately 6 millimeters or 1/4 inch).
- E – Evolving: Any changes in the mole’s size, shape, color, or elevation should be closely monitored.
If you notice any of these signs, it’s crucial to seek professional evaluation promptly. Early detection can significantly improve treatment outcomes.
GentleCure™ is a Surgery-Free Treatment for Basal Cell Skin Cancer
If you’re facing a basal cell skin cancer diagnosis, you do have treatment options. Image-Guided Superficial Radiotherapy (Image-Guided SRT) is the surgery-free gold standard for skin cancer treatment, proving to be just as effective as Mohs surgery and without cutting or surgical scarring. Learn how it works and reach out to our Skin Cancer Information Specialists at 855-936-4411 for more information.